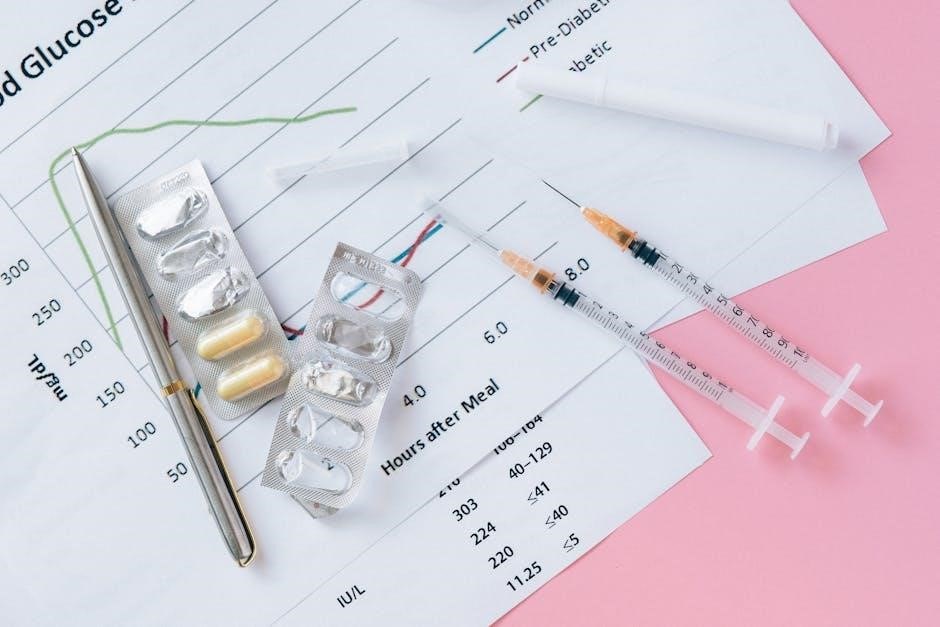
Insulin charts are essential tools for organizing and managing diabetes treatment plans‚ providing clear visuals for blood glucose levels‚ insulin doses‚ and administration times to ensure consistency and accuracy.
1.1 Importance of Insulin Charts for Diabetes Management
Insulin charts are vital for effective diabetes management‚ helping patients and healthcare providers track blood glucose levels‚ insulin doses‚ and administration times. They provide a clear‚ organized format to visualize trends‚ ensuring accurate adjustments to treatment plans. By minimizing dosing errors and improving adherence‚ insulin charts enhance glycemic control‚ reducing the risk of complications like hypoglycemia or hyperglycemia. Regular use of these charts supports personalized therapy‚ enabling tailored adjustments based on blood sugar patterns‚ meals‚ and physical activity‚ ultimately improving overall diabetes outcomes and patient well-being.
1.2 Overview of Insulin Chart PDFs
Insulin chart PDFs are downloadable templates designed to help patients and caregivers track blood glucose levels‚ insulin doses‚ and administration schedules. These charts often include sections for recording blood sugar readings‚ insulin units administered‚ and meal times. They may also provide space for noting any hypoglycemic episodes or adjustments to treatment plans. Many insulin chart PDFs are customizable‚ allowing users to tailor the format to their specific needs. These tools are widely available online and serve as practical resources for maintaining organized and accurate diabetes management records‚ ensuring better glycemic control and communication with healthcare providers;
Types of Insulin
Understanding insulin types is crucial for effective diabetes management. Insulin varieties include rapid-acting‚ short-acting‚ intermediate‚ long-acting‚ and combination insulins‚ each with distinct onset‚ peak‚ and duration profiles.
2.1 Rapid-Acting Insulin
Rapid-acting insulin‚ such as Humalog (lispro) and NovoLog (aspart)‚ begins working within 10-15 minutes‚ peaks in 1-3 hours‚ and lasts about 4 hours. It is administered before meals to control blood sugar spikes. This type is ideal for managing postprandial glucose levels and offers flexibility in dosing. Its fast onset mimics natural insulin secretion‚ making it a popular choice for basal-bolus regimens. Patients often use it via pens or pumps for convenience. Rapid-acting insulin is crucial for achieving tight glycemic control and reducing A1c levels effectively.
2.2 Short-Acting Insulin
Short-acting insulin‚ such as Humulin R and Novolin R‚ begins working in 30 minutes‚ peaks between 2-4 hours‚ and lasts 6-8 hours. It is typically administered before meals to manage blood sugar spikes. This insulin type is often used in combination with intermediate-acting insulins for basal coverage. Short-acting insulin can be mixed with intermediate-acting insulins but not with rapid-acting types. It is commonly prescribed for type 1 diabetes and for type 2 diabetes when oral medications are insufficient. Monitoring for hypoglycemia and weight gain is essential when using short-acting insulin.
2.3 Intermediate-Acting Insulin
Intermediate-acting insulin‚ such as NPH (Neutral Protamine Hagedorn)‚ begins working within 1-2 hours‚ peaks between 4-12 hours‚ and lasts 12-18 hours. It is typically administered twice daily‚ in the morning and evening‚ or before bedtime. This insulin type provides basal coverage and is often combined with rapid- or short-acting insulins for mealtime glucose control.
Intermediate-acting insulin is suitable for patients requiring longer duration of action. Typical dosing ranges from 0.5-1.0 units/kg/day‚ with adjustments based on blood glucose monitoring. Consistent administration times are crucial for maintaining glucose control and minimizing side effects like hypoglycemia and weight gain.
2.4 Long-Acting Insulin
Long-acting insulin‚ such as glargine (Lantus) and detemir (Levemir)‚ provides a smooth‚ basal insulin supply with minimal peaks. It is designed to mimic natural pancreatic insulin secretion‚ lasting 12-24 hours‚ depending on the type. These insulins are typically administered once or twice daily‚ offering flexibility for patients.
Long-acting insulin helps maintain consistent blood glucose levels between meals and during sleep. It is often prescribed for patients with type 1 diabetes and some with type 2 diabetes. Dosing is adjusted based on fasting blood glucose levels and overall glucose control goals.
2.5 Combination Insulin
Combination insulin products blend rapid- or short-acting insulin with intermediate- or long-acting insulin‚ offering both mealtime and basal glucose control in one injection. These insulins‚ such as NovoLog Mix 70/30 or Humalog Mix 75/25‚ are designed to simplify treatment regimens for patients who require both types of insulin action.
They are typically administered before meals to manage postprandial glucose spikes while providing background insulin coverage. Combination insulins are often prescribed for individuals with type 2 diabetes or those transitioning from oral medications to insulin therapy‚ helping to reduce the number of daily injections and improve adherence to treatment plans.
Insulin Dosing and Schedules
Insulin dosing and schedules are personalized plans outlining the timing‚ type‚ and amount of insulin to manage blood glucose levels effectively throughout the day.
3.1 Basal Insulin Dosing
3.2 Bolus Insulin Dosing
Bolus insulin dosing is designed to manage blood glucose spikes after meals. It is typically administered before eating and is calculated based on the current blood glucose level‚ carbohydrate intake‚ and insulin sensitivity. Rapid-acting or short-acting insulins like aspart or lispro are commonly used. Dosing may include a correction factor to lower high blood sugar and a carbohydrate ratio to cover meal-related increases. For example‚ 1 unit of insulin might cover 15 grams of carbohydrates or reduce blood glucose by 50 mg/dL. Proper bolus dosing ensures post-meal glucose levels remain within target ranges‚ preventing hyperglycemia and its complications.
3.3 Sliding Scale Insulin Dosing
Sliding scale insulin dosing is a flexible treatment approach where insulin doses are adjusted based on current blood glucose levels. It is often used in hospital settings or for patients with fluctuating glucose levels. The regimen typically outlines specific insulin doses for different blood glucose ranges. For example‚ a blood glucose level of 70-110 mg/dL might require no insulin‚ while 111-150 mg/dL could require 2 units‚ and 151-200 mg/dL might need 4 units. This method allows healthcare providers to tailor insulin administration dynamically‚ ensuring timely and effective glucose control without adhering to a fixed dosing schedule.

Blood Glucose Monitoring and Insulin Adjustment
Regular blood glucose monitoring helps tailor insulin doses to individual needs‚ ensuring optimal glucose control and minimizing risks of hypoglycemia or hyperglycemia through timely adjustments.
4.1 Blood Sugar Levels and Insulin Sensitivity
Blood sugar levels play a crucial role in determining insulin sensitivity‚ which varies among individuals. Monitoring glucose levels helps identify patterns and adjust insulin doses accordingly.
Higher blood sugar levels may indicate reduced insulin sensitivity‚ requiring larger doses to achieve optimal control.
Tools like sliding scale insulin charts provide structured guidance for dose adjustments based on glucose readings.
Understanding this relationship is key to preventing hypoglycemia and hyperglycemia‚ ensuring safe and effective diabetes management.
Regular monitoring and tailored adjustments minimize risks and improve overall metabolic health.
4.2 Adjusting Insulin Doses Based on Blood Glucose Readings
Adjusting insulin doses based on blood glucose readings is critical for maintaining glycemic control. High blood sugar levels may require increased doses‚ while low levels may need reduction.
Using a sliding scale insulin chart‚ healthcare providers can determine appropriate doses for different glucose ranges.
For example‚ a reading of 151-200 mg/dL might require 4 units of rapid-acting insulin‚ while levels below 70 mg/dL demand hypoglycemia treatment.
Regular monitoring and documentation help refine insulin regimens‚ ensuring safety and effectiveness.
Consistency in adjustments prevents complications and improves long-term diabetes management.

Insulin Chart Examples
Examples include sliding scale charts‚ blood sugar charts with A1c levels‚ and insulin peak charts‚ providing visual guides for insulin dosing and blood glucose regulation.
5.1 Sample Sliding Scale Insulin Chart
A sliding scale insulin chart outlines the dosage of insulin based on blood glucose levels. For example‚ a blood sugar range of 125-150 mg/dL may require 2 units of insulin‚ while 151-200 mg/dL might need 4 units. This chart is customizable to individual patient needs and is widely used in clinical settings to manage glucose levels effectively. It provides a clear‚ visual guide for healthcare providers to adjust insulin doses accordingly‚ ensuring precise treatment plans. The chart is often included in insulin chart PDFs for easy reference and implementation.
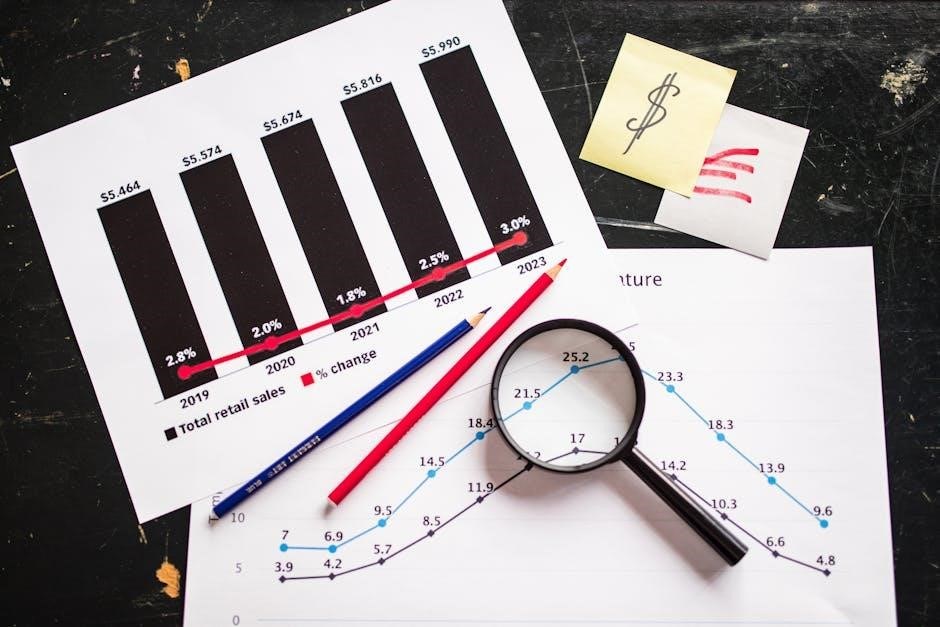
5.2 Blood Sugar Chart with A1c Levels
A blood sugar chart with A1c levels is a comprehensive tool that correlates daily glucose readings with long-term glycemic control. It displays blood glucose ranges alongside corresponding A1c percentages‚ helping patients and healthcare providers track progress. For example‚ blood sugar levels of 125-150 mg/dL may align with an A1c of 6-7%. This chart is often included in insulin chart PDFs to provide a visual reference for managing glycemic targets and adjusting treatment plans. It simplifies understanding the relationship between daily glucose monitoring and long-term diabetes control‚ aiding in personalized therapy adjustments.
5.3 Insulin Peak Chart
An insulin peak chart visually represents the onset‚ peak‚ and duration of various insulin types‚ helping to optimize dosing schedules. It illustrates how rapid-acting insulins like Humalog peak within 1-3 hours‚ while long-acting insulins like Lantus provide a flat‚ prolonged effect. This chart is invaluable for aligning insulin administration with blood glucose patterns‚ preventing hypoglycemia‚ and enhancing glycemic control. By understanding the peak action times‚ users can adjust their insulin therapy to match daily activities and meals‚ ensuring more effective diabetes management. It is often included in insulin chart PDFs for easy reference and personalized care.

Calculating Insulin Doses
Insulin doses are calculated using formulas based on weight and insulin sensitivity‚ helping personalize treatment plans and adjust based on blood glucose levels for effective management.
6.1 Insulin Sensitivity Factor (Correction Factor)
The Insulin Sensitivity Factor (ISF)‚ or correction factor‚ determines how much insulin is needed to lower blood glucose by a specific amount. It is typically calculated as 1500 divided by the Total Daily Dose (TDD) of insulin for rapid-acting insulin. This factor varies among individuals and can be influenced by factors like diabetes type‚ duration‚ and insulin resistance. For example‚ a sensitivity factor of 50 means 1 unit of insulin lowers blood glucose by 50 mg/dL. Regular monitoring and adjustments are crucial to ensure accurate dosing and avoid hypoglycemia or hyperglycemia. Healthcare providers often fine-tune this factor based on blood glucose trends.
6.2 Total Daily Dose (TDD) of Insulin
The Total Daily Dose (TDD) of insulin is the sum of all insulin doses taken in a 24-hour period‚ including basal and bolus insulins. It is calculated by adding up the units of insulin administered throughout the day. For example‚ if a patient takes 20 units of basal insulin and 30 units of bolus insulin‚ their TDD is 50 units. Factors like insulin sensitivity‚ meal patterns‚ and blood glucose levels influence TDD. Adjustments are often needed to maintain target blood glucose levels and prevent complications. TDD is a critical metric for personalized diabetes management.
Insulin Therapy and Management
Insulin therapy involves personalized treatment plans to manage blood glucose levels‚ incorporating basal‚ bolus‚ and combination insulins. Proper dosing‚ timing‚ and lifestyle adjustments are critical for effectiveness.
7.1 Insulin Resistance and Therapy
Insulin resistance occurs when the body’s cells do not respond effectively to insulin‚ leading to elevated blood glucose levels. This condition often requires adjustments in therapy‚ such as increasing insulin doses or adding medications like metformin. Somatostatin analogs can reduce insulin resistance but may also impair insulin secretion‚ potentially causing hyperglycemia. Managing insulin resistance involves lifestyle changes‚ including diet and exercise‚ alongside optimized insulin regimens. Clinical studies highlight the importance of personalized treatment plans to address insulin resistance effectively‚ balancing glucose control with potential side effects like weight gain.
7.2 Metformin and Insulin Therapy
Metformin is often prescribed alongside insulin therapy to enhance glucose control‚ particularly in type 2 diabetes. It works by reducing hepatic glucose production and improving insulin sensitivity. When combined with insulin‚ metformin can lower blood sugar levels without causing significant weight gain‚ a common side effect of insulin therapy alone. This dual approach helps achieve better glycemic control and reduces the risk of diabetes-related complications. Clinical studies suggest that metformin complements insulin therapy by addressing insulin resistance and promoting more efficient glucose utilization in the body. This combination is a cornerstone in managing advanced type 2 diabetes cases effectively.
7.3 Obesity and Insulin Therapy
Obesity significantly impacts insulin therapy‚ as excess body weight often leads to insulin resistance‚ requiring higher doses to achieve glucose control. Weight gain is a common side effect of insulin therapy‚ creating a cycle that worsens insulin resistance. Managing blood glucose in obese patients can be challenging‚ as larger doses may be needed to overcome resistance. However‚ certain types of insulin‚ such as glargine‚ may help mitigate weight gain. Clinicians must carefully balance insulin dosing to avoid hypoglycemia while addressing the unique needs of obese patients‚ often incorporating lifestyle interventions to enhance treatment outcomes.

Insulin Products Comparison
Insulin products vary by brand‚ formulary status‚ concentration‚ and administration‚ with detailed charts comparing onset‚ peak‚ and duration of action to guide treatment decisions effectively.
8.1 Brand Name and Formulary Status
Insulin products are compared by brand name and formulary status‚ with charts detailing coverage and availability. Brand names like Humalog‚ Toujeo‚ and others are listed alongside their formulary status‚ indicating whether they are preferred or non-preferred options. This comparison helps healthcare providers and patients make informed decisions based on insurance coverage and treatment accessibility. Formulary status can significantly impact cost and availability‚ making it a critical factor in insulin therapy selection. Charts often highlight brand-specific details‚ ensuring clarity in choosing the most suitable insulin product for individual patient needs. This information aids in optimizing treatment plans and cost-effectiveness.
8.2 Concentration and Administration
Insulin charts detail the concentration of insulin products‚ such as 100 units/mL‚ 200 units/mL‚ or 300 units/mL‚ ensuring proper dosing. Administration methods are also highlighted‚ including subcutaneous injections using pens‚ syringes‚ or vials. Charts specify whether insulin can be mixed with other types or if it requires separate administration. Timing guidelines‚ such as administering insulin before meals or at bedtime‚ are provided to optimize glucose control. This section helps healthcare providers and patients understand the correct usage and handling of insulin products‚ ensuring safe and effective therapy. Proper administration is key to achieving desired glycemic outcomes.
8.3 Onset‚ Peak‚ and Duration of Action
Insulin charts provide detailed information on the onset‚ peak‚ and duration of action for various insulin types. Rapid-acting insulins begin working within 10-20 minutes‚ peak in 1-3 hours‚ and last 3-5 hours. Long-acting insulins like glargine and detemir have a slower onset‚ typically within 1-2 hours‚ with a flat peak and duration of 12-24 hours or more. Understanding these profiles helps tailor insulin regimens to individual needs‚ ensuring optimal blood glucose control. This data is critical for adjusting doses and timing to match lifestyle and glucose patterns effectively. Accurate timing prevents hyperglycemia and hypoglycemia‚ enhancing overall diabetes management.

Patient Education and Safety
Patient education is crucial for safe insulin use‚ focusing on proper injection techniques‚ hypoglycemia prevention‚ and recognizing symptoms. Regular monitoring and dose adjustments ensure therapy effectiveness and minimize risks.
9.1 Avoiding Dosing Errors
Avoiding insulin dosing errors is critical to prevent hypoglycemia and hyperglycemia. Using insulin charts and sliding scale guidelines helps ensure accurate dose calculations. Clear communication between healthcare providers and patients is essential. Always verify the insulin type‚ concentration‚ and administration timing. Double-checking doses before administration reduces mistakes. Patient education on proper injection techniques and adherence to prescribed regimens minimizes errors. Regular monitoring of blood glucose levels and documentation in insulin charts further enhances safety. Always refer to updated clinical guidelines and pharmacy resources‚ such as PharMerica’s insulin drug chart‚ for standardized protocols.
9.2 Hypoglycemia Treatment and Prevention
Hypoglycemia‚ or low blood sugar‚ is a common side effect of insulin therapy. Symptoms include sweating‚ shaking‚ confusion‚ and dizziness. Immediate treatment involves consuming fast-acting carbohydrates like glucose tablets or juice. Severe cases may require glucagon administration. Prevention strategies include regular blood glucose monitoring‚ adjusting insulin doses based on glucose readings‚ and maintaining consistent meal times. Patient education on recognizing symptoms and carrying emergency supplies is crucial. Insulin charts help track glucose patterns and guide dose adjustments to minimize hypoglycemic episodes‚ ensuring safer and more effective diabetes management.
9.3 Weight Gain and Insulin Therapy
Weight gain is a common side effect of insulin therapy‚ particularly with long-acting insulins. This occurs due to increased insulin levels‚ which promote fat storage. Patients often notice weight gain in the abdominal area‚ which can increase the risk of complications like cardiovascular disease. Monitoring food intake and physical activity is crucial to manage weight. Adjusting insulin doses or switching to weight-neutral insulins‚ such as GLP-1 receptor agonists‚ may help mitigate weight gain. Regular follow-ups with healthcare providers are essential to address this issue effectively and maintain overall health.

References and Citations
References include clinical studies‚ guidelines‚ and author contributions‚ citing sources like ОО Голоунина (2021) and МВ Шестакова (2017)‚ with 9 citations‚ providing credible insights.
10.1 Clinical Studies and Guidelines
Clinical studies emphasize the importance of insulin therapy in managing blood glucose levels‚ with references to works by ОО Голоунина (2021) and МВ Шестакова (2017). These studies highlight the efficacy of basal and bolus insulin regimens‚ particularly in type 1 diabetes‚ and the role of insulin sensitivity in dose adjustments. Guidelines from organizations like the University Medical Center pharmacy provide structured approaches for sliding-scale insulin dosing‚ ensuring safe and effective glycaemic control. These resources underscore the importance of personalized treatment plans and regular monitoring to optimize insulin therapy outcomes.
10.2 Author Contributions and Acknowledgments
The authors extend gratitude to ОО Голоунина and МВ Шестакова for their insightful research on insulin resistance and therapy. Their studies‚ cited in 2021 and 2017‚ provided foundational data for this article. Special thanks to PharMerica for their comprehensive insulin drug chart‚ which served as a key reference. Contributions from clinical experts and researchers have enriched the content‚ ensuring accuracy and relevance. Their work has significantly advanced understanding of insulin management and dosing strategies‚ benefiting both healthcare professionals and patients.